Postpartum depression is one of the major challenges that is faced by new parents. Often dubbed as “the thief that steals motherhood”. It is a form of mental health issue that is most commonly seen in women after childbirth.
Also called, postnatal depression (PPD), it is a complex mix of physical, emotional, and behavioral changes that occur in some women after giving birth. It is a form of major depression that is associated with childbirth. Typically, it develops within the first few weeks after delivery, but it can also arise later, up to a year postpartum.
Although postpartum depression (PPD) has been recognized since 400 BC, it gained substantial attention only about fifty years ago. Numerous research endeavors and reviews have been conducted over the past decades to delve into various aspects of PPD.
Approximately 13% to 19% of women who have recently given birth experience PPD, making it a prevalent postnatal health concern affecting 520,000 to 760,000 women annually in the United States. This makes postpartum depression as having the highest morbidity rates in the country.
Apart from affecting the mother, PPD’s timing also has consequences on the child, impacting maternal-child interaction and attachment. Children of mothers with PPD may experience sleeping and eating problems, along with behavioral difficulties.
But what does it feel like and how does it manifest?
Looking Into The Symptoms Of Postpartum Depression
Postpartum depression (PPD) encompasses a range of symptoms that affect women after childbirth. It is crucial to recognize these signs for early detection and appropriate intervention.
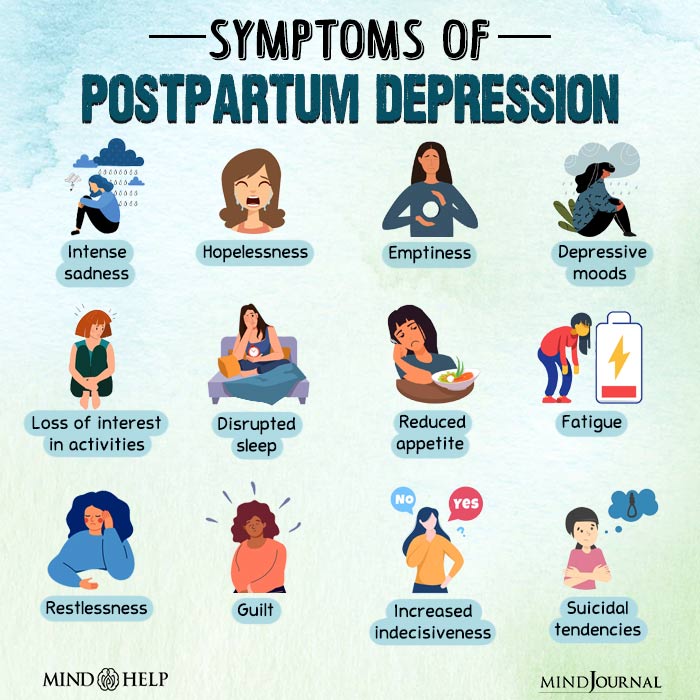
The symptoms can are:
1. The Cloud of Persistent Sadness:
Think about the fact that you feel a constant cloud of sadness hanging over your head. It is one of the most common symptoms of postpartum depression. It’s not merely “baby blues” but the more profound, prolonged feeling of hopelessness that tends to ruin every moment- including those precious moments with your new baby.
2. The Challenge of Bonding:
This idea that every mom instantly bonds with her baby is a fable. In the case of PPD, this connection can feel even harder to establish leaving moms feeling guilty or like they’re failing as mothers. Always remember that it doesn’t mean you don’t love your baby or are incapable as their mother.
3. On an Emotional Rollercoaster:
It’s like being on an emotional rollercoaster with PPD; one minute you are fine, and the next minute, you are irritable or become extremely agitated by nothing in particular. It’s as if your emotions are on a hair-trigger and sometimes this extends to an overwhelming fear of accidentally hurting your little one.
4. Battling Guilt and Worthlessness:
PPD has a way of making you feel worthless or perpetually guilty inside your mind. This is another sign where mothers blame themselves for things they couldn’t change; remember these feelings do not reflect your parenting accurately.
5. When Sleep Doesn’t Equal Rest:
Sleeping issues or constant fatigue? That’s how PPD manifests itself physically. Additionally, apart from struggling with emotions – muscle pain, headaches or just always feeling exhausted which doesn’t make taking care of a newborn any easier.
6. Pulling Away from the World:
You may withdraw from the world around you due to postpartum depression leading to increased feelings of isolation in some cases for example absence from family get-togethers or not going out with friends anymore. It’s really difficult however staying connected is important because a simple phone call or meeting for coffee can make a big difference.
7. When PPD Goes Beyond:
In its most severe forms, PPD can also resemble other mental health issues such as anxiety, OCD, panic attacks, etc. It’s a web of emotions and reactions that are complicated and need to be understood and worked through gently.
If you or someone you know is experiencing these symptoms of postpartum depression, it’s important to seek help. Post-partum depression is not “one size fits all” and affects every mom differently. It is not an indication of weakness but rather it signifies the need for support as well as understanding.
Recognizing these symptoms and understanding their causes is crucial for early intervention and effective support. Hence, we request you to read more on the common causes of postpartum depression in new mothers.
Postpartum Depression Causes That You Are Overlooking
That being said, motherhood is often a very joyous event but for some women, it can also come along with certain difficulties. The causes of postpartum depression (PPD) are still being investigated.
The following are some of the common postpartum depression causes according to researchers:
1. Emotions on a rollercoaster:
Being a new mom can feel like riding an emotional roller coaster. However, sometimes, the feelings you have about your baby, battles with unhappiness or nervousness in the past and even traumatic incidents like rape could make this journey more bumpy.
It’s important to acknowledge these emotions and realize that they may impact your mental health after giving birth.
2. When Pregnancy Gets Tough:
Pregnancy isn’t always smooth sailing. Complications like emergency C-sections or unexpected hospital stays can be stressful. Also, concerns about your baby’s health, like premature birth or low weight, add to this stress. These difficulties don’t just affect your physical health; they can also impact your mental wellbeing.
3. The Power of Support:
The popular quote “It takes a village to raise a child” is true, especially when discussing your mental health after pregnancy. A lack of support combined with unfriendly environments such as domestic violence can take a toll on you. Interestingly, some habits such as smoking during pregnancy are also involved. It is important to look for help and have a safe environment for this period.
4. Lifestyle factors:
Your daily activities have a bigger impact than you would think. These everyday selections ranging from what you eat to how much sleep or exercise can affect your moods. Focusing on your sleep patterns and nutritional needs, like getting enough Vitamin B6 can be useful in managing mood after delivery.
5. Hormonal influences:
Once you give birth to your child, there is huge hormone shift in your system. After pregnancy, two critical hormones namely estradiol and progesterone fall abruptly. This sudden change may be quite a shock to your body system.
Oxytocin and prolactin which are crucial for milk production and let-down reflex, also play a role in PPD. Low oxytocin levels are associated with both PPD and early weaning. Research shows that Oxytocin, often dubbed the ‘love hormone,’ is central to bonding and maternal behaviors.
Recognizing your risk factors can allow healthcare professionals to develop treatment plans for your disease. Based on these factors healthcare professionals will be able to provide you with the right postpartum depression treatment options.
Exploring Postpartum Depression Treatment Options
Several postpartum depression treatment options are available for new moms and families. You need to explore the different treatment options available before you start your prognosis.
Each option provides its unique benefits and challenges, let’s take a look:
1. The Go-To Treatment of using SSRIs
When it comes to treating moderate to severe PPD, Selective Serotonin Reuptake Inhibitors (SSRIs) are often the first line of defense.
These medications have shown promise in clinical trials for effectively managing PPD symptoms. It’s worth noting that while SSRIs are a common choice, it’s crucial to have a conversation with your healthcare provider about what’s best for you.
2. Exploring Alternate Medical Options
While there’s a wealth of information about SSRIs, other antidepressants like Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) are also on the radar, though with less extensive research backing. Medications like Venlafaxine and Desvenlafaxine have been suggested in some studies to help with PPD symptoms.
3. Traditional Antidepressants in the Mix
Tricyclic antidepressants (TCAs) and Monoamine Oxidase Inhibitors (MAOIs) also find their place in the discussion about PPD treatment. However, the evidence here is more limited, making it all the more important to have a tailored treatment plan based on your specific needs and medical history.
4. Preventing PPD From Happening Again
If you’ve had PPD before, the possibility of it recurring can be a concern. SSRIs and TCAs are often considered for prevention, but as with treatment, more research is needed to fully understand their effectiveness in this area.
5. Holistic Approaches Beyond Medications
Many women prefer exploring psychotherapy or complementary health practices, especially during pregnancy. These alternatives can be appealing for their perceived benefits and often align more closely with personal preferences and lifestyles.
6. ECT and Other Interventions In Severe Cases
For more severe or recurring cases of PPD, treatments like electroconvulsive therapy (ECT) might be considered. While this might sound intimidating, ECT has shown higher response rates for severe PPD and postpartum psychosis. Newer techniques, like transcranial magnetic stimulation, are also being explored.
Remember, treating PPD is a highly personal journey. What works for one may not work for another, so it’s crucial to discuss all your options with your healthcare provider. As research continues to advance, we hope to see more and more effective treatments becoming available.
Always remember, you’re not alone in this, and there are resources and support available to help you through.
But what if you are the partner in the relationship? What should you do when your partner is going through postpartum depression? Continue reading to get hands-on postpartum depression tips for spouses.
Key Postpartum Depression Tips For Spouses
One can hardly overemphasize the importance of spousal support in postpartum depression (PPD). It is a road that needs comprehension, endurance, and empathy for one’s spouse going through postpartum depression.
Given below are some key tips on postpartum depression for spouses, which have been borrowed from the experiences and advice of others who have been through such situations.
1. Understanding the Condition:
It is vital to understand what it means to have PPD. Speaking directly with your partner’s medical team will give you invaluable insights into her condition, how severe her symptoms are, and her progress in recovery. This knowledge removes any uncertainty and stress for both of you.
2. Encourage Self-Care:
Encourage activities that make your partner happy and refreshed. These may include exercise, hobbies, socialization, or making sure they take care of their basic hygiene like showering.
3. Offer Unprompted Support:
Sometimes supporting means doing something without being asked. That could mean taking care of the baby so she can have alone time or doing more around home with them.
4. Focusing on Your Partner:
Make sure you concentrate on how your partner feels. Ask about their labor experience, what they look forward to after delivery, whether they are healthy as well as if they have any worries or not to redirect attention from the baby toward women.
5. Be a Source of Emotional Support:
This is an opportunity for you to agree with her feelings and let her know that you understand the things she is going through are difficult for her. Showing them that you see hope for better days ahead and acknowledging how serious their situation is may be enough for a major change.
6. Seeking Your Support:
Supporting a partner with PPD can be challenging, and partners need to seek their support when needed. This could involve talking to a family physician, spending time with friends and family, or seeking therapy.
7. Be Patient and Kind:
Remember how challenging it is for your partner to go through postpartum depression every day. Being patient, kind, and understanding can help them feel more supported and less alone.
These insights provide a starting point for spouses wanting to support their partners through postpartum depression. Each couple’s journey is unique and what works for one may not work for another couple. The most important thing is being available, supportive and understanding when professional help is required.
A Word From Mind Family
While concluding our discussion about Postpartum Depression (PPD), it is worth noting that this issue is taken seriously as it affects new moms and their families. It’s not just some momentary feeling of sadness; for ladies after delivery, it’s a big deal that can be tough.
We went over what causes PPD, how it feels, and ways to help treat it. This knowledge is paramount for PPD mothers and also their family members, especially partners.
You play a very important role when you are a partner to someone with PPD. In such cases, being there for them even without asking for help can make a whole lot of difference in their lives knowing that they are going through a difficult time. However, do not forget that you also have a responsibility to take care of yourself and seek support when necessary.
PPD may be difficult but no mother should face it alone. It needs the involvement of everybody to fight against it starting with doctors, friends, and family members. At Mind Family we believe that when we hold hands together we will surely overcome difficult times like PPD.
If you want to know more about PPD and how to support your family, you can always talk to doctors and mental health experts. You’re not alone, and there’s always help available.
Frequently Asked Questions (FAQs)
1. What is postpartum depression?
Postpartum depression (PPD) is a mental health issue commonly experienced by women after childbirth, affecting both physical and emotional well-being. Often referred to as “the thief that steals motherhood,” it involves a complex mix of symptoms associated with major depression.
2. What are the symptoms of postpartum depression?
PPD manifests through various symptoms, including a persistent cloud of sadness, challenges in bonding with the baby, emotional rollercoasters, feelings of guilt and worthlessness, physical manifestations like trouble sleeping and exhaustion, withdrawing from the world, and, in severe cases, overlapping symptoms with other mental health issues.
3. What are the common postpartum depression causes?
Postpartum depression causes are multifaceted. Emotional factors include past battles with sadness or anxiety, traumatic experiences like sexual abuse, and feelings about the baby. Pregnancy complications, lack of support, exposure to domestic violence, smoking during pregnancy, and lifestyle choices also contribute. Hormonal shifts after childbirth play a significant role.
4. What are the options for postpartum depression treatment?
Treatment options for PPD include pharmaceutical interventions such as SSRIs, SNRIs, TCAs, and MAOIs. Psychotherapies, complementary health practices, and neuromodulatory interventions like electroconvulsive therapy (ECT) are explored. Personalized approaches, including self-care, lifestyle adjustments, and seeking emotional support, are essential components.
5. What are some postpartum depression tips for husbands?
Supporting a partner through PPD requires understanding, patience, and compassion. Tips for spouses include educating themselves about PPD, encouraging self-care, offering unprompted support, focusing on the partner’s feelings, being a source of emotional support, promoting seeking professional help when needed and being patient and kind. Each journey is unique, requiring tailored support and understanding.







Leave a Reply